Identification of Drug-Related Problems (DRPs) in Chronic Kidney Disease Patients at the Inpatient Unit of Dr. Sitanala Hospital, Tangerang, 2019-2021
DOI:
https://doi.org/10.36733/medicamento.v10i2.7006Keywords:
Chronic renal failure,, drug related problems, renal functionAbstract
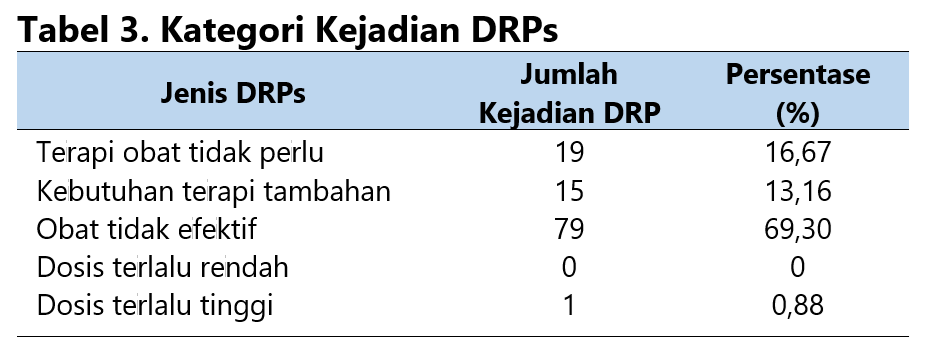
Chronic kidney disease (CKD) is characterized by the gradual decline of kidney function over one year or more. The primary functions of the kidneys include maintaining fluid balance, regulating blood electrolyte levels, ensuring acid-base homeostasis, and removing waste products and excess electrolytes. Drug-related problems (DRPs) are medication-related issues that can negatively impact patients' quality of life. This study aims to determine the prevalence of DRPs in CKD patients treated at Dr. Sitanala Hospital, Tangerang, during 2019-2021. This descriptive study used retrospective data collection, presenting the results as percentages. Ninety-two (92) patients met the inclusion criteria, with a gender distribution of 48 males (52.17%) and 44 females (47.83%). The most common age group was 56-65, accounting for 28 cases (30.43%). The prevalence of DRPs in hospitalized CKD patients was found to be 89 cases (96.74%), with the following breakdown: 19 cases (16.67%) of unnecessary drug therapy (TOTP), 15 cases (18%) requiring additional therapy (KTT), 79 cases (69.3%) of ineffective drugs (OTE), and 1 case (0.88%) of drugs with too high a dose (DTT), while no cases of drugs with too low a dose (DTR) were identified.
References
Menteri Kesehatan Republik Indonesia. Peraturan Menteri Kesehatan Republik Indonesia Nomor 72 Tahun 2016 tentang Standar Pelayanan Kefarmasian di Rumah Sakit. Published online 2016:63.
Riskesdas T. Laporan Nasional Riskesdas 2018. Lembaga Penerbit Badan Penelitian dan Pengembangan Kesehatan (LPB); 2019. http://labdata.litbang.kemkes.go.id/images/download/laporan/RKD/2018/Laporan_Nasional_RKD2018_FINAL.pdf
Shabaka A, Cases-Corona C, Fernandez-Juarez G. Therapeutic Insights in Chronic Kidney Disease Progression. Frontiers in Medicine. 2021;8(February):1-12. doi:10.3389/fmed.2021.645187
Sari F, Annisa N, Rijai. Kajian Pengobatan Pasien Gagal Ginjal Kronik di Rumah Sakit Samarinda Medika Citra (SMC). ProsidingFarmasiUnmulAcId. 2017;(November):7-8.
Kher KK, Greenbaum LA, Schnaper HW. Clinical Pediatric Nephrology. Third Edit. (Kher K, Schnaper HW, Greenbaum LA, eds.). CRC Press; 2016. doi:10.1201/9781315382319
Haryanti IAP, Nisa K. Terapi Konservatif dan Terapi Pengganti Ginjal sebagai Penatalaksanaan pada Gagal Ginjal Kronik. Majority. 2015;4:49-54.
Luntungan P, Tjitrosantoso H, Yamlean PVY. Potensi Drug Related Problem (DRPs) Pada Pasien Gagal Ginjal di Rawat Inap RSUP Prof.DR.R.D.Kandau Manado. PHARMACON Jurnal Ilmiah Farmasi. 2016;5(3):23-33.
Calvo-Salazar RA, David M, Zapata-Mesa MI, Rodríguez-Naranjo CM, Valencia-Acosta NY. Drug-related problems causing hospital admissions in the emergency rooms at of high complexity hospital. Farmacia Hospitalaria. 2018;42(6):228-233. https://www.sciencedirect.com/science/article/pii/S1130634323007419
Juwita DA, Rachmaini F, Abdillah R, Meliani M. Drugs Related Problems (DRPs) Pada Pasien Penyakit Ginjal Kronik (PGK) Di RSUP Dr. M. Djamil. Jurnal Sains Farmasi & Klinis. 2022;9(sup):184. doi:10.25077/jsfk.9.sup.184-189.2022
Adiana S, Maulina D. Klasifikasi Permasalahan Terkait Obat (Drug Related Problem/DRPs): Review. Indonesian Journal of Health Science. 2022;2(2):54-58. doi:10.54957/ijhs.v2i2.238
Kamil I, Agustina R, Wahid A. Gambaran Tingkat Kecemasan Pasien Gagal Ginjal Kronik Yang Menjalani Hemodialisis Di RSUD Ulin Banjarmasin. Dinamika Kesehatan. 2018;9(2):366-377.
Hödlmoser S, Winkelmayer WC, Zee J, et al. Sex differences in chronic kidney disease awareness among US adults, 1999 to 2018. Kronenberg F, ed. PLOS ONE. 2020;15(12):e0243431. doi:10.1371/journal.pone.0243431
Pranandari R, Supadi W. Faktor Risiko Gagal Ginjal Kronik Di Unit Hemodialisis Rsud Wates Kulon Progo. Majalah Farmaseutik. 2015;11(2):316-320.
Fogo AB, Cohen AH, Colvin RB, Jennette JC, Alpers CE. Nephrosclerosis and Hypertension. In: Fundamentals of Renal Pathology. Springer Berlin Heidelberg; 2014:125-133. doi:10.1007/978-3-642-39080-7_10
James PA, Oparil S, Carter BL, et al. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults. JAMA. 2014;311(5):507. doi:10.1001/jama.2013.284427
Yuniarti W. Anemia pada Pasien Gagal Ginjal Kronik. Journal Health & Science : Gorontalo Journal Health and Science Community. 2021;5(2):341-347. doi:10.35971/gojhes.v5i2.11632
Palliative Care Guidelines: Renal Palliative Care. Symptom control in patients with chronic kidney disease/ renal impairment. 2013;(August):1-5.
Alvionita, Welinda Dyah Ayu MAM. Pengaruh Penggunaan Asam Folat Terhadap Kadar Hemoglobin Pasien Penyakit Ginjal Kronik Yang Menjalani. J Trop Pharm Chem 2016. 2016;3(3):179-184.
Dipiro JT, Tabelt RL, Yee GC, Matzkee GR, Wells BG PL. Pharmacotherapy Handbook. Seventh Ed. McGraw-Hill Companies; 2008. doi:10.1036/007147899X
DeBellis RJ, Smith BS, Cawley PA, Burniske GM. Drug dosing in critically ill patients with renal failure: A pharmacokinetic approach. Journal of Intensive Care Medicine. 2000;15(6):273-313. doi:10.1046/j.1525-1489.2000.00273.x
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Sefi Megawati, Syifa Sopiahani, Nuriyatul Fathonah

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.

















