Quality of prescribing in patients with hypertension: A narrative review
DOI:
https://doi.org/10.36733/medicamento.v10i1.7659Keywords:
hypertension, prescribing, quality, reviewAbstract
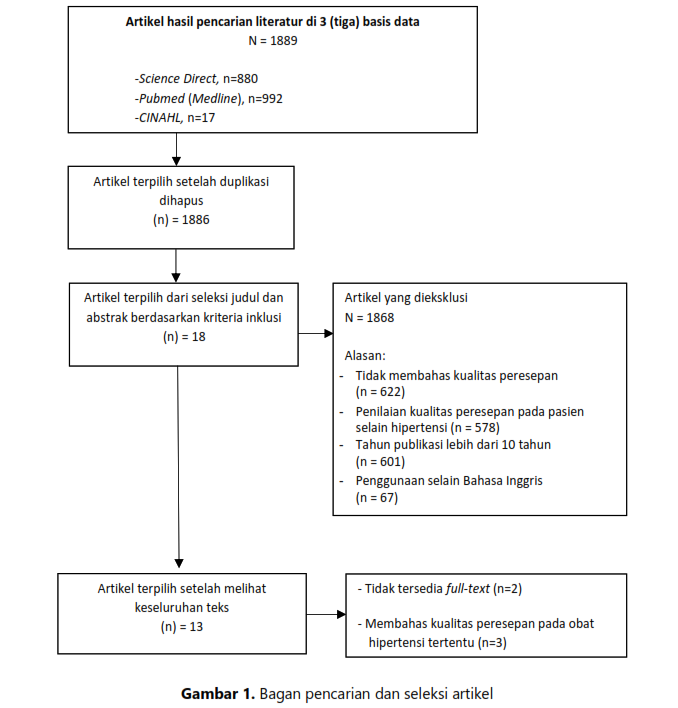
Assessing the rational use of medicines or prescription quality is essential in any health system. However, data on the quality of prescribing in patients with hypertension is currently lacking. Hence, this review aimed to identify prescribing quality indicators in patients with hypertension and understand the results. A narrative review was conducted to include literature searching in three databases, including PubMed (Medline), Science Direct, and CINAHL, using keywords and Boolean Logic as follows: “(hypertension OR antihypertensive drugs OR antihypertensive medication OR antihypertensive agent) AND (quality prescription OR inappropriate prescribing OR potentially inappropriate medication OR rational prescribing)”. As a result, a total of 1889 articles were obtained. The articles were then selected based on inclusion and exclusion criteria in which 13 articles were included in this review. Based on the extracted data, explicit as well as implicit frameworks have been used to assess the quality of prescribing in patients with hypertension. Explicit approaches compared patient prescription versus guidelines (n=7 articles) or lists of potentially inappropriate use of medicines (n=3 articles). The implicit framework assessed patient prescription using two tools, including the prescription Quality Index (PQI) – 22 indicators (n=2 articles), and the prescription quality checklist – four indicators (n=1 article). The results of the quality assessment on the prescriptions showed that prescriptions categorized as good quality were between 40-80%. While varied levels of inappropriate selection of antihypertensive therapy were reported (0-65%). In addition, more than 30% of patients with hypertension experienced Potentially Inappropriate Medication (PIM); thus, prescribing among patients with hypertension needs to be optimized.
References
World Health Organisation (WHO). The pursuit of responsible use of medicines: sharing and learning from country experiences. Geneva: WHO; 2012.
Lima MG, Álvares J, Junior AAG, et al. Indicators related to the rational use of medicines and its associated factors. Rev Saude Publica. 2017;51 Suppl 2:23s. https://doi.org/10.11606/S1518-8787.2017051007137
Hodkinson A, Tyler N, Ashcroft DM, et al. Preventable medication harm across health care settings: a systematic review and meta-analysis. BMC Med. 2020;18:13. https://doi.org/10.1186/s12916-020-01774-9
Fujita K, Moles R, Chen T. Quality indicators for responsible use of medicines: a systematic review. BMJ Open. 2018;8:e020437. doi:10.1136/bmjopen-2017-020437.
Mills K, Bundy J, Kelly T, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441-450.
Smeulers M, Verweij L, Maaskant J, et al. Quality indicators for safe medication preparation and administration: A systematic review. PLoS One. 2015;10:e0122695.
Sadeghi B, Farhoudi M, Hajebrahimi S, et al. 2015. A systematic review on clinical indicators, their types and codification processes. Journal of Clinical Research & Governance. 2015;4:1-9.
Catumbela E, Certal V, Freitas A, et al. Definition of a core set of quality indicators for the assessment of HIV/AIDS clinical care: a systematic review. BMC Health Serv Res. 2013.13:236.
Krishnapillai V, Nair S, Anand T, et al. Quality of medical prescriptions in diabetes and hypertension management in Kerala and its associated factors. BMC Public Health. 2020;20:193.
Paradkar S, Sinha S. Drug utilization among hypertensive patients in the outpatient department of medicine in a tertiary care hospital A cross-sectional study. Clinical and Experimental Hypertension. 2018 40: 150-154.
Suthar J, Patel V. Assessment of quality of prescribing in patients of hypertension at a primary and secondary health care facilities using the Prescription Quality Index (PQI) tool. Indian Journal of Pharmacology. 2014;46:480-484.
Suthar J, Patel V, Vaishnav B. Quality of prescribing for hypertension and bronchial asthma at a tertiary health care facility, India using Prescription Quality Index tool. Journal of Basic and Clinical Pharmacy. 2015; 6:1-6. doi: 10.4103/0976-0105.145759.
Tandon V, Sharma S, Mahajan S, et al. Antihypertensive drug prescription patterns, rationality, and adherence to Joint National Committee-7 hypertension treatment guidelines among Indian postmenopausal women. Journal of Mid-life Health. 2014;5:78-83.
Varankantham V, Sailoo A, Bharatraj D. Antihypertensive Prescription Pattern and Compliance to JNC 7 and JNC 8 at Tertiary Care Government Hospital, Hyderabad, India: A cross-sectional Retrospective Study. Hospital Pharmacy. 2018;53:107-112. doi: 10.1177/0018578717738080.
Alkaabi M, Rabbani S, Rao P, et al. Evaluation of antihypertensive prescriptions for rationality and adherence to treatment guidlelines: An experience from United Arab Emirates. Clinical Epidemiology and Global Health. 2020;8:764-769.
Al Khaja K, Isa H, Veeramuthu S, et al. Potentially Inappropriate Prescribing in Older Adults with Hypertension or Diabetes Mellitus and Hypertension at Primary Care Setting in Bahrain. Medical Principles and Practice. 2018;27:241-249. doi: 10.1159/000488055.
Alhawassi T, Krass I, Pont L. Prevalence, management and control of hypertension in older adults on admission to hospital. Saudi Pharmaceutical Journal. 2017;25:1201-1207.
Falster M, Buckley N, Brieger D, et al. Antihypertensive polytherapy in Australia: Prevalence of inappropriate combinations, 2013-2018. Journal of Hypertension. 2020;38:1586-1592.
Basopo P, Mujasi P. To what extent do prescribing practices for hypertension in the private sector in Zimbabwe follow the national treatment guidelines? An analysis of insurance medical claims. Journal of Pharmaceutical Policy and Practice. 2017;10:37.
Marquez P. Potentially inappropriate antihypertensive prescriptions to elderly patients: Results of a prospective, observational study. Drugs Aging. 2017;34:453-466. doi: 10.1007/s40266-017-0452-z.
Bazargan M, Smith J, O King E. Potentially inappropriate medication use among hypertensive older African-American adults. BMC Geriatrics. 2018;18:238.
Guyatt G, Rennie D, Meade M, et al. Users' guides to the medical literature: Essentials of evidence-based clinical practice. New York: McGraw Hill Education; 2015.
Downloads
Submitted
Accepted
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Devina Erawati Santoso, Yosi Irawati Wibowo, Adji Prayitno Setiadi

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.





















